The Tooth Extraction Survival Guide!
 There is reason why the phrase “like pulling teeth” is so popular. Getting a tooth taken out is one of those dental experiences you don’t forget. Whether it’s the pain / discomfort of the procedure, the noises, or having a missing tooth afterwards, there is no part of this that is fun. Having a tooth pulled is usually a last resort when the tooth can no longer be fixed. All that said, knowing what to expect beforehand and being prepared can make the experience significantly better for you. Read on to learn everything you need to know in order to make the best of your tooth pulling experience.
There is reason why the phrase “like pulling teeth” is so popular. Getting a tooth taken out is one of those dental experiences you don’t forget. Whether it’s the pain / discomfort of the procedure, the noises, or having a missing tooth afterwards, there is no part of this that is fun. Having a tooth pulled is usually a last resort when the tooth can no longer be fixed. All that said, knowing what to expect beforehand and being prepared can make the experience significantly better for you. Read on to learn everything you need to know in order to make the best of your tooth pulling experience.
Before The Procedure
Consider if you want sedation for the extraction/s. Sedation can range from taking a light sedative beforehand or laughing gas all the way up to full general anesthesia where you won’t remember anything. Most general dentists are able to offer light sedatives or laughing gas while you usually have to go to an oral surgeon for IV sedation or general anesthesia. If you are having multiple extractions, especially wisdom teeth that are impacted, IV sedation or general anesthesia can make the process significantly easier and less traumatic for you.
Take Ibuprofen before having an extraction and it will lessen the pain afterwards significantly. Several studies have backed this up. This assumes that you don’t have any health problems that make it so you can’t take NSAIDs (mostly GI or kidney problems). You’ll also want to be a little more careful if you’re on blood thinners. Ibuprofen can make you bleed slightly more. This isn’t a problem for most people but can make things more difficult if you are already of blood thinners. Ask your dentist or oral surgeon if you’re concerned.
The Procedure
During an extraction the dentist will numb the tooth and then proceed to slowly loosen the tooth with several instruments until it can be removed. Sometimes this process takes 30 seconds and other times it can take an hour, depending on the specifics of the situation. For especially difficult extractions the dentist may need to section the tooth into several pieces or remove bone around it to allow the tooth to come out.
There are several types of extractions…
- Simple extraction – This is when the dentist or oral surgeon is able to remove the tooth without needing to section or remove bone. Recovery from these types of extractions are the easiest lasting a couple of days.
- Surgical extraction – In these cases the dentist or oral surgeon has to remove bone and/or section the tooth in order to remove it. Recovery from these types of extractions takes a little longer with pain lasting anywhere from 2 days to several weeks.
- Soft tissue, Partial and Full bony impacted teeth extractions – In these cases the teeth are covered either by gum tissue or bone and they take the most effort to remove. Recovery in these cases usually takes the longest.
A tooth that is very sensitive or infected can be very difficult to numb even with the best of techniques.
What You Can Expect to Feel and Hear
During a tooth extraction, you will usually feel a lot of pressure as the tooth is slowly loosened. This sensation can be a bit uncomfortable but should not be sharply painful. Many people have a hard time differentiating between the pressure and pain. Usually this is because they aren’t sure what expect and the pressure makes them worried. Knowing this going in can help you to relax about the procedure. Expect a lot of pressure.
You’ll also hear some noises. These noises can range from small popping sounds, to cracking, to the sound of the drill if the tooth needs to be sectioned or bone removed. Don’t be worried if you hear this. It is a perfectly normal part of the process. The sounds sound a lot louder to you than what other people would hear.
When the dentist uses the forceps to start removing the tooth, occasionally they’ll slip off the tooth or break pieces off. This can also be scary if you’re not expecting it. Most teeth that need an extraction have quite a bit of the tooth broken or are about to break. Part of the process is that the dentist has to find a solid area of the tooth to grip on and this can take a couple of tries.
Common Complications of Extractions
Sinus exposure – The roots of upper molars are in very close proximity to your maxillary sinuses. If a small hole is noticed after the extraction your dentist will usually place a small
Dry socket – A dry socket forms when the blood clot is lost in the extraction site. This causes significant pain starting 3-5 days after the tooth is removed. Read below in “After The Extraction” for tips on avoiding a dry socket. A dry socket isn’t dangerous, but is very painful, usually worse than before the tooth came out. A dry socket will heal on it’s own in anywhere from a week to several weeks without treatment. Your dentist can also place a medication in the socket to help reduce some of the pain.
Bone or tooth fragments – Small pieces of bone or tooth can be dislodged and will slowly work their way out over time. Most of the time you’ll notice a small, slightly painful area where the tooth came out. You’ll then notice a small hard piece in the area. When it has come through the gums enough to grab it, you can pull it out and it’ll heal quickly. Your dentist can also do this for you if you’re squeamish or it is too painful.
Swelling – This most commonly happens with difficult extractions. You can have swelling right around the area where the tooth came out or you can have swelling that extends all the way onto your face. Impacted wisdom tooth extractions are famous for giving people the “chipmunk” look with large swollen cheeks. Ice packs for the first day will help lessen this.
Root tip left in place – Some teeth have very skinny, curved root tips. During the extraction these can break off and be very difficult to retrieve. If your dentist decides that the risk of removing them is too great, they’ll often leave these in place. Most of the time they don’t cause any problems long term.
Infection – This is the least likely of all the complications. It is most common with teeth that were abscessed prior to the extraction. If they infection doesn’t resolve after a couple of weeks or if you continue to have significant swelling, pus drainage, or pain your dentist may go back in to drain the area and put you on an antibiotic.
After The Extraction
Smoking, sucking on straws, very hot foods or liquids, or birth control medication all can raise your risk of getting a dry socket afterwards which is very painful. Dry sockets are most common with difficult extractions of lower wisdom teeth and molars.
Continue taking your pain medication as prescribed for the first couple of days so you can stay ahead of the pain. Only taking it when it hurts will lead to a bad cycle of pain. You usually need to do this for the first 48-72 after the extraction. Beyond that point, the pain will decrease significantly.
Avoid any heavy labor or exercise for the first 24 hours.
Eat a soft diet for the first day or two. You’ll also want to avoid anything excessively spicy or acidic as these can cause the area to burn. After the first couple of days you can go back to a normal diet, just being careful to avoid anything getting stuck in the socket.
You can start rinsing gently with warm salt water 24 hours after the tooth removed. Don’t do this too vigorously.
If you’re a smoker, avoid smoking as long as you are possibly able to. Three days should be a minimum and longer is better if you can. The heat and chemicals from the cigarette delay healing and can increase your risk of a dry socket.
Some discharge and bad taste are normal for about a week after the extraction. This will slowly decrease with time.
The extraction site will usually develop a white or grey coating over top of it. Ulcers right around the area aren’t unusual either. This is normal and nothing to be concerned about. The gum tissue will slowly heal over this area over the course of the next several weeks to months.
Long Term Consequences Of Having A Tooth Removed
If you pull a tooth, the teeth behind it tend to start falling forward over the course of several years.
If the tooth below it no longer hits on anything, it will start to erupt (move) upwards over time.
An extraction can cause you to lose additional bone on the tooth in front or behind it. This can compromise that tooth over time.
A tooth in front or behind the extraction can also become more sensitive. This can be a result of either the trauma of the extraction or surfaces of the tooth being exposed that weren’t exposed before. This sensitivity will decrease after several weeks to months.
You’ll continue to slowly lose bone in the area unless you have an implant placed. Bone loss over time can make it more difficult to fit dentures or place implants in the future.
Root Canals
There are a couple of different situations in which a tooth needs a root canal…
- Tooth decay extends into the nerve space – Once the nerve has been exposed, it is very unlikely to recover on it’s own.
- The nerve is in the process of dying (very painful) – Every time a tooth is traumatized (from bumps or dental work) it pushes it a little more towards dying. When the nerve starts to die it usually causes severe sensitivity to hot and cold as well as a constant throbbing pain that is bad enough to wake you up at night.
- The nerve is dead – The final stage the nerve gets to is when it dies. When it dies all of the tissue inside the tooth starts to become infected which eventually leads to a dental abscess. If the infection gets out of control you can get swelling and pain in the area. In very rare cases the infection can spread to other parts of the body. Antibiotics can help reduce some of these symptoms but they will come back unless a root canal is done to remove all of the infected tissue inside the tooth.
During a root canal the dentist or endodontist (root canal specialist) cleans out the entire nerve space of the tooth with several sets of metal files. She or he then rinses out the inside of the tooth with several different solutions including sodium hypochlorite (bleach), chlorhexidine, and/or EDTA. After the entire space has been cleaned it is filled in with a plastic type material known as gutta percha.
After a root canal you can expect the tooth to be somewhat sore. This soreness can be be very limited while other times it lasts for several months. Additionally after a root canal, the tooth usually ends up needing a crown on it. The root canal severely weakens the tooth and it has a relatively high risk of breaking catastrophically. If you do get a root canal and your dentist recommends a crown, make sure you get that done within a couple of months or you will have wasted all the money you spent on the root canal.
Crowns
 When a tooth is broken or decay is pretty large, the next option after a filling is a crown (or occasionally an onlay which is similar). The picture to the right is a classic example of a tooth that needs a crown. It has a very large filling which is broken.
When a tooth is broken or decay is pretty large, the next option after a filling is a crown (or occasionally an onlay which is similar). The picture to the right is a classic example of a tooth that needs a crown. It has a very large filling which is broken.
So what actually happens when you get a crown?
When a dentist prepares your tooth for a crown he or she removes about a millimeter all the way around the tooth and about a millimeter and a half on top. The crown is made to slide on to the tooth and restore it’s natural shape. Because the crown covers the entire tooth it prevents any additional breaks. The crown is cemented on to the tooth and the tooth generally acts and functions like a normal tooth again.
I took some pictures of a larger than life model to give you an idea of how the crown procedure works.
 Final crown being put in place
Final crown being put in place
Crown Materials
There are a lot of different types of materials that crowns are made out of. The following are the most common…
Gold
These crowns aren’t actually made entirely out of gold but a combination of gold and other metals. Gold itself is too soft so other metals are added to improve it’s strength. Gold crowns are especially useful on your very back molars where there is little room to prepare the tooth. Gold can be made thinner than any other material for a crown. The only downside to a gold crown is what it looks like which is another reason it is normally only used for back teeth.
Porcelain Fused to Metal (PFM)
PFM crowns were the gold standard in crowns for many many years. They are made so that the inside of the crown is made of metal and the outside is covered with porcelain. They are very durable but occasionally the porcelain will break off of the metal. They look very natural except in some cases where the metal shows through. I try to avoid these types of crowns on front teeth for that reason.
Porcelain Fused to Zirconia (PFZ)
These are mostly used for bridges on front teeth to provide good strength but also good esthetics.
Emax (lithium disilicate)
This is a relatively new material. It is made entirely out of porcelain and is very strong. It also can be made to look very natural. One of it’s biggest advantages is that it can be chemically bonded to your tooth which makes it very unlikely to come off.
Zirconia
This last type of crown is the strongest type of crown that is white. Zirconia can be pounded with a hammer and not break. It doesn’t look as natural as Emax crowns and is mostly used on back teeth.
Can A Tooth That Needs A Crown Be Filled Instead?
Many people ask, isn’t there any way you can fill my tooth instead? The answer, as with many other things in dentistry, is that teeth that need crowns can be filled but it really isn’t a great idea. If your dentist recommended a crown, it is very likely that the tooth will break at some point in the future without one. Sometimes this break can be repairable and sometimes the tooth will break catastrophically and you end up having to have it extracted.
Bridges
Bridges are similar to crowns but used for a different purpose. Bridges are used to replace a missing tooth by connecting the teeth on either side of the space with teeth that are prepared for crowns. Bridges used to be a very popular option for replacing teeth but with the success of implants they’ve become the back-up option if an implant won’t work. One of the biggest problems with bridges is that you have to cut down the teeth on both side of the space, even if there is nothing wrong with them. It is basically a three tooth solution to a one tooth problem. Most bridges on back teeth are PFM or Zirconia while bridges on front teeth are oftentimes PFZ or emax.
Missing tooth in between two other teeth
Bridge (all connected) placed over both teeth to replace missing tooth
Final bridge in place
There are several unique challenges with bridges. Food tends to get stuck underneath it and you can’t normally floss around it. The easiest way to keep it clean is with a Waterpik. Other options include floss threaders, superfloss, or proxabrushes to clean under the bridge. See our section on floss reviews for more information.
Fillings
The dentist will numb your tooth and use a dental drill to remove the area of the tooth that is decayed. Many people ask if they can have the filling done without being numb because they are so scared of shots. My personal opinion is that if the decay is small enough that you don’t need to be numbed, then it is probably not at the point that it needs a filling. I have had patients who are exceptions to this but it is pretty unusual. The decayed area is usually soft and stained and the dentist removes all of this. This halts the decay process and also provides a solid foundation to put the filling material on.
There are several major types of filling material…
Amalgam
Amalgam is the oldest of the filling materials. It has been in use since the early 1800’s and has proven over that time period to be extremely durable and easy to place. It is made of a combination of silver, tin, copper, and mercury. Amalgams have become controversial recently due to concerns about the mercury content and it’s effect on the brain, especially the developing brain. Despite significant long term studies that have demonstrated no related health issues as far as they can tell, it has nonetheless begun to be phased out in most areas.
Composite
Composite resin fillings are one of the types of “white” fillings. Composite fillings as we know them today were first developed in the 1980’s and have undergone some significant changes and upgrades in the time since. Composites are made of a mixture of plastic and glass particles. The biggest challenge with composite fillings is that in order to bond them to the tooth, there must be perfect isolation from any saliva, unlike amalgam and glass ionomer fillings. There also tends to be a bit more sensitivity following these fillings than with other types. This has been reduced with better bonding systems over the years but can still be a pretty significant problem. Composite fillings have had some controversy of their own in the last several years when it was discovered that bisphenol-A (BPA) can cause certain types of health problems. Most composite fillings have a small amount of BPA that is released over time. The good news is that the amount released is miniscule (approximately 1/1000 the amount that you receive from other sources daily) and is very unlikely to cause any health problems.
Glass Ionomer
Glass ionomer is another type of “white” filling material that is used for dental cements as well as some types of fillings. Glass ionomer is formed from a reaction of silica glass particles and an acid. It isn’t a strong material but does have the benefit of bonding to teeth on it’s own and releasing fluoride to help prevent future decay. These fillings are generally used on baby teeth as well as when there is decay on the root surfaces of teeth.
Once the fillings have been placed your dentist will smooth them down and make sure your teeth come together correctly. After having fillings done you can expect some sensitivity and soreness for several days to several weeks afterwards. Occasionally you will need the dentist to adjust your “bite” after the numbness has worn off and you can feel exactly how you are biting together.
Routine Cleanings
 Most people believe that the important part of the dental cleaning is when the dental hygienist uses the minty paste and polishes their teeth. Believe it or not, that is actually the least important part of the whole process! Lets run through all the different things that your dental hygienist does during your cleaning visit.
Most people believe that the important part of the dental cleaning is when the dental hygienist uses the minty paste and polishes their teeth. Believe it or not, that is actually the least important part of the whole process! Lets run through all the different things that your dental hygienist does during your cleaning visit.
Updating your medical history
Did you know that the health of the mouth has a direct link with many other health conditions? Your hygienist makes sure your health history is updated so we can take those things into consideration when recommending any sort of dental treatment.
Checking the periodontal health of your teeth
Most hygienists will check all around your teeth for signs of gum disease at least once a year.
Updating your x-rays
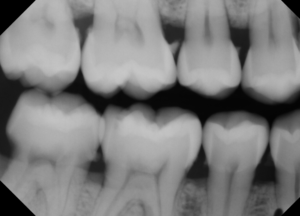
New patients usually have a comprehensive set of x-rays and thereafter once every 3-5 years. For returning patients 4 bitewing x-rays are taken once a year to check for cavities in between the teeth as well any signs of gum disease.
Scaling your teeth
This is when they take those sharp instruments and remove any hard build-up on your teeth. This is one of the more important parts of your cleaning visit. Those hard deposits on your teeth, also known as calculus, are nearly impossible for you to remove yourself. If these areas aren’t cleaned off it can lead to gum disease and bone loss around your teeth. If your hygienist only polishes and doesn’t scale, you’re likely not getting a thorough cleaning (unless you’re the 0.1% of people who have no calculus build-up at all).
Polishing your teeth
So we’re back to polishing your teeth. Polishing simply removes a lot of the soft plaque and stain on your teeth. Studies have shown very little clinical benefit to this part of the cleaning but it is done mostly so that your teeth feel nice and clean when you leave. Believe it or not, you can get this exact same feeling simply by doing a really thorough brushing. A good electric toothbrush works even better.
Scaling and Root Planing (“Deep Cleaning”)
 Article Updated February 24th, 2017.
Article Updated February 24th, 2017.
So it’s been a couple of years since your last dental cleaning and you go into the dental office. They take a bunch of x-rays and stick a sharp little probe all around your gums all the while calling out random numbers. Then they sit you up and explain to you that you have “periodontal disease” or “gum disease”. They’re going to need to do scaling and root planing! Is this for real?
What is going on?
Let’s break it down. First the x-rays. Here is a patient of mine who hadn’t been to the dentist in quite a few years. This is actually one of the worst cases of build-up that I’ve ever seen but it gives you a good picture of what can happen. See those white projections on the side of the teeth? That is called tartar or calculus (not the math kind either!). Dental plaque that sits on the tooth too long calcifies and becomes hard. When it gets to this point it is almost impossible for you to remove yourself, especially when it is under the gum-line. These areas attract more bacteria and plaque which just continues to build up. Your body attacks the area and you start losing bone around the teeth! Eventually this can lead to the teeth getting so loose that they fall out! I’ve literally had patient’s come in with their teeth in their hand.
Pockets and Probings
Now next let’s talk about all those numbers. When they going around each tooth and calling out numbers they are actually measuring how deep the “pockets around the teeth are. Bone loss and inflammation will generally cause higher numbers. Normal is 1-3 mm, 4 is borderline, and anything over 5 mm indicates periodontal disease. When you get to numbers like 7-10 you’re looking at severe bone destruction and the need for more intensive treatment. The really terrible part is that generally bone around your teeth can’t be regrown except in very limited circumstances.
The following pictures are from my favorite tooth model of periodontal disease. One side of the mouth shows normal bone around the teeth while the other side shows build-up around the teeth as well as bone loss which is especially severe around the back molar teeth. When we go in to do scaling and root planing on patients, this is exactly the kind of thing we see! Please get treatment done and don’t let it progress until you lose your teeth or affect your overall health!
Gum Disease… A Silent Tooth Killer
Periodontal disease is much like heart disease or diabetes in that it silently causes damage and you generally don’t know there is a problem until it is too late. Usually the only signs early signs are bleeding and puffy gums. If any other part of your body easily bled, you would likely be worried and would see a physician. It should be the same with bleeding gums. Bleeding with brushing is not normal and should be addressed!
It seems to me that gum disease is one of the least understood problems from a patient’s point of view. I think it is hard because it isn’t something you can usually see until it is far too late. Major bone loss has to occur before you notice gums receding and loose teeth. Like we talked about before, it is a lot like heart disease in that respect. A lot of people don’t ever realize they have heart disease until they have a heart attack. Would you ever tell your physician that you don’t think they should treat your heart disease because it isn’t hurting right now? Of course not. You don’t want to wait until it causes a problem. You want to treat it aggressively so that it doesn’t become a problem. It is exactly the same for gum disease. Sure, gum disease won’t directly kill you (but it can contribute to some other diseases that can) but losing your teeth early can cause a huge drop in overall quality of life.
There are also a lot of myths out there surrounding gum disease. We hear a lot of them from our patients including “It doesn’t hurt so I don’t need treatment”, “My gums aren’t bleeding so I can’t have gum disease”, “My whole family lost their teeth so I will too”, or “I brush my teeth all the time so there isn’t any way I have gum disease”. Dr. Nemeth, a world renowned Periodontist (gum disease specialist), has a nice article on his website answering some of these gum disease myths… Common Myths About Gum Disease.
Taking care of periodontal disease is also important to overall health. Periodontal disease is linked to heart disease, diabetes, and preterm births. See our section on the Mouth-Body connection for information on this link.
OK, so what do we do about this? How do we stop it? Prevent it?
The first line of treatment is generally known as scaling and root planing, which many people call a deep cleaning. What your dentist or hygienist will do is numb the entire area and then go under the gum-line and clean out all that build-up and smooth the surfaces. They will use a combination of hand instruments and ultrasonic instruments that break up the tartar and disrupt the bacteria. For most people this will allow the area to heal and get back on track.
For people with mild to moderate gum disease, scaling and root planing along with a change in oral hygiene habits will be enough to get their mouth healthy again. For people with more severe disease or other factors that complicate the situation, they may need additional treatment at a periodontist. This can include surgery, laser treatments, and/or antibiotics.
Now, it’s really important to realize that this isn’t the entire fix. You’ve got to change your habits and how you clean your teeth to maintain this condition. If you go back to minimal brushing and no flossing, you’ll be back in this same situation in a couple of years. Brushing for two minutes, twice a day, and flossing daily is the single most important thing you can do to keep periodontal disease away and maintain your teeth for a lifetime.
If you’re a smoker, I highly recommend working on cutting back or quitting. Smoking is one of the biggest risk factors for gum disease.
Why Fix Baby Teeth?
 I get a lot of questions from parents when I recommend treatment on baby teeth. They usually wonder why we want to fix the baby teeth when they are just going to fall out eventually anyway. As it stands, there are actually a lot of good reasons to want to fix baby teeth.
I get a lot of questions from parents when I recommend treatment on baby teeth. They usually wonder why we want to fix the baby teeth when they are just going to fall out eventually anyway. As it stands, there are actually a lot of good reasons to want to fix baby teeth.
#1: Baby teeth hold the space for the permanent teeth. If these teeth are lost too early there won’t be space for the permanent tooth to come in and it will either be impacted or come in in the wrong direction leading to terrible crowding. Severely crowded teeth can be very difficult and expensive to fix when the child is older.
#2: Cavities develop rapidly in baby teeth – Enamel is very thin in baby teeth compared to permanent teeth. If we don’t fix these cavities they can very quickly become large cavities that cause pain and infection. Infection can be dangerous. There have been many cases of dental infections that have gotten out of control and the child died.
#3: Some baby teeth will be there until they are 12 years old! Many parents don’t realize that kids still have baby teeth at that age. If they develop a cavity at age 5 or 6, you can bet that cavity will become very large leading to loss of the tooth way too early if not treated.
#4: Teeth, especially front ones, are critical for developing proper speech patterns.
#5: Missing teeth make it very difficult to chew food. Children have far fewer surfaces to chew on in the back than adults do and this can impact their nutrition. I always find it very sad when I see a child who has lost multiple molars in the back and must go without them for years.
Accidents
 If you’ve got kids, it’s very likely you’re eventually going to see some sort of dental trauma! I’d estimate that at least a third of kids have had some sort of dental accident. This can range from minor bruises / cuts to completely breaking a tooth or knocking it out. The key thing is to be prepared and know what to do in case any of these scenarios happen!
If you’ve got kids, it’s very likely you’re eventually going to see some sort of dental trauma! I’d estimate that at least a third of kids have had some sort of dental accident. This can range from minor bruises / cuts to completely breaking a tooth or knocking it out. The key thing is to be prepared and know what to do in case any of these scenarios happen!
The usual scenario is that the kids are playing, you hear a big bump, and your kid comes running to you with blood all over their face! It’s easy to freak out and panic! Try to stay calm, collected, and take a step by step approach to figuring out what happened.
First get a wet rag or paper towel to clean up the blood. Blood in the mouth tends to look worse than elsewhere because it mixes with saliva, goes everywhere, and looks like much more than there actually is. Once you get it cleaned up you can figure out where it is coming from.
Secondly, if someone else is around, send them to get some children’s ibuprofen. You’ll want to have the kid drink this as soon as possible in order to get the painkilling effects going. If no one else is around, figure out what is going on first, then give them some ibuprofen.
Once you’ve figured out where the bleeding is coming from you can figure out what to do next. Here are the most likely scenarios.
They bit into or through their lip
Depending on the extent of the wound, they may or may not need stitches. The general rule is that if the wound stays closed on it’s own (for example if they just bit straight into their lip without any tearing, etc) then it doesn’t need stitches. Any wound that doesn’t stay closed on it’s own or won’t stop bleeding will likely need stitches. If you don’t know, put something in the area for them to apply pressure and take them to your ER or dentist’s office. Pressure is the most important thing needed to stop the bleeding.
They hit their teeth which are bleeding but not loose
In this case, you really don’t need to do anything. Most of the time these teeth will heal on their own. Some significant soreness and sensitivity is pretty normal for about the first week or two afterwards. It’s not terribly unusual for the traumatized tooth to eventually turn gray. The grayness is similar to a bruise. Most of the time these gray teeth are just fine. Occasionally traumatized teeth will become abscessed after some time. Your child may complain of pain with the tooth and you might notice something that looks like a pimple on the gums right above the tooth. You should see your dentist as soon as possible if you notice either of these things.
They hit their teeth which are bleeding and loose
If the teeth are still in their original position and only slightly loose, no treatment is generally necessary. A lot of times these teeth will heal and they will tighten up again. Pretty much everything I discussed in the last section applies to these teeth.
On the other hand if the teeth are displaced out of their original position you’ll want to see a dentist as soon as possible. If it is a baby tooth, these teeth will need to be removed. A permanent tooth should be moved back into it’s original position as soon as possible and a light splint placed on the tooth to stabilize it. If you’re able to push it back into it’s original position at home before seeing the dentist, even better. Many of these permanent teeth will end up needing a root canal.
They hit their teeth and chipped one
This happens pretty rarely with baby teeth as they tend to get knocked out rather than broken due to the soft bone around them. This happens much more often in the permanent teeth, especially the front ones in the first couple of years after they come in. I can’t even count how many kids I’ve seen who’ve chipped their front teeth biking, playing sports, or running into walls. It happens all the time so don’t feel bad if it happens to your child! Small chips can generally be repaired with a filling while very large chips that involve the nerve of the tooth usually end up needing a root canal. If you’re able to find the piece that chipped off, bring this in to the dentist as they can sometimes bond the fragment back in place.
They hit their teeth and knocked one out entirely
If it is baby tooth that has been knocked out, there isn’t a whole lot to do! Baby teeth should never be put back in place if they’ve been knocked out. This can damage the permanent tooth underneath. Put it under their pillow and tell them the tooth fairy gives extra money for teeth that are knocked out.
Permanent teeth on the other hand need immediate attention. If you’re able to put it back in place immediately, this is the absolute best thing you can do. Rinse any debris off of it as gently as possible. Do not scrub or rub it. Push back in place. If you’re not comfortable doing this, put the tooth in a glass of milk and get to your dentist as quickly as possible. Success rates doing this drop rapidly after an hour so you want it treated as soon as possible. If you wait more than a couple of hours, there is no chance of successfully replanting the tooth and you’ll have to start looking at replacement options.
Thumb and Finger Sucking

As you can imagine, it presents a significant esthetic as well as functional problem!
Breaking the child of the habit can be very difficult, especially if it has been a comfort for many years. In many cases you won’t be able to break the habit until the child is ready despite your best efforts. Some different options include throwing away their pacifier, putting a terrible tasting gel on their fingers, bribing them with a prize for 20 days of not doing it, and as a last resort, a dental appliance that sits behind their front teeth and doesn’t allow them to put fingers in. At a minimum you want this habit broken before they start losing baby teeth and getting permanent teeth in. I’d recommend starting to break the habit at age 2 if you’re able as this will minimize any damage done. If you can’t break the habit and are noticing significant change in their teeth, start saving up for braces because they will likely be in them a while.
When Do Teeth Come In / Fall Out?
 Kids seem to be constantly getting teeth in or losing them for about the first twelve years of life! For first time parents this can be a really confusing and stressful process. In my experience, parents who have already been through it with an older child tend to worry quite a bit less! The important thing to remember is that this is an entirely normal and natural process that happens! Some discomfort is perfectly normal and no matter what you do, the process usually takes care of itself (with some exceptions).
Kids seem to be constantly getting teeth in or losing them for about the first twelve years of life! For first time parents this can be a really confusing and stressful process. In my experience, parents who have already been through it with an older child tend to worry quite a bit less! The important thing to remember is that this is an entirely normal and natural process that happens! Some discomfort is perfectly normal and no matter what you do, the process usually takes care of itself (with some exceptions).
Lets talk first about getting those initial teeth in. The rule of thumb is the first teeth start coming in around age 7 months and they’ll get another 4 teeth in every 4 months for a total of 20 teeth when they’re done right around 2 to 2 1/2 years old. While these are averages, there is a huge amount of variation between kids, not only in when the teeth come in, but also the order. Don’t worry if your child is getting them in faster / slower than other kids. This doesn’t necessarily mean there is any problem. The usual order is the front four teeth will come in first, then their first molars, then canines / eye teeth, and lastly their second molars. Good thing those second molars come in last because they are the biggest and most uncomfortable to break through! Once they’re all in you don’t have to worry about teeth coming in / out for about 3 more years! No more drooling, biting things, and general crankiness! Yay! Baby orajel and the occasional use of Tylenol for pain is just about all you need for these years.
Your next milestone is right around 6 years old. Again this is wildly variable. I’ve seen kids as young as 5 starting the process and some kids don’t have anything happen until age 7. This will usually start with the two bottom front teeth starting to get loose and some new (really big!) molars coming up right behind their last baby teeth. These new molars (first permanent molars or six year molars) are permanent teeth and you want to make sure they take extra special care of them because they are some of the most important teeth they will get! Oftentimes the permanent teeth in front will come in behind the baby teeth and for a while they’ll have a double row of “shark teeth”. Again this is totally normal! I literally can’t count how many times I’ve seen this. I tell the kids they look awesome with their “shark teeth” and send them off and invariably they end up losing them in next couple of weeks and the permanent teeth move into the right spot. In pretty quick succession they’ll lose the front four teeth on the top and the bottom and then they’ll have another break for a couple of years.
Right around age 10 they’ll start losing teeth again and this will continue until around age 12 when all the baby teeth are gone and they get their second molars (twelve year molars) in the very back. Hooray! You’ve got another 6 year break!
Around age 18, if they have wisdom teeth, they’ll start to come in. Many people’s wisdom teeth will be partially impacted and won’t come in all the way. If there is any concern as to their positioning or space available for them I’d highly recommend they are taken out. Wisdom teeth are one of the most common problem areas for adults who haven’t had them out.